Please Read This : Changes in Hospital Insurance Coverage for Cancer Treatments
Apr 26, 2024 3:43 am
Hey ,
Starting from April 1st, all hospital insurance plans will align with MOH’s regulations, covering only approved drugs listed in the Cancer Drug List (CDL) managed by MOH.
Therefore, any cancer treatment not listed in the CDL will no longer be covered by your hospital insurance. However, if you have the rider, there will be additional coverage to cover treatment costs not in the CDL.
Please reach out if you are unsure about what I am referring to.
Another key change to note is that if a patient is prescribed more than one drug on the CDL list for the same cancer treatment for one primary cancer, the claim limit will be pegged to the highest individual claim limit of the drug in the combination.
In short, if Drug A has a claim limit of $2,500 and Drug B has a claim limit of $800, only the highest-cost drug can be claimed, not the sum of all claim limits for individual drugs.
Starting April 1st, MOH introduced another regulation for Multiple Primary Cancers. This is defined as two or more cancers arising from different sites and/or different histology or morphology groups.
The claim limits will be the sum of the highest cancer drug treatment limit among the claimable treatments received for each primary cancer per month.
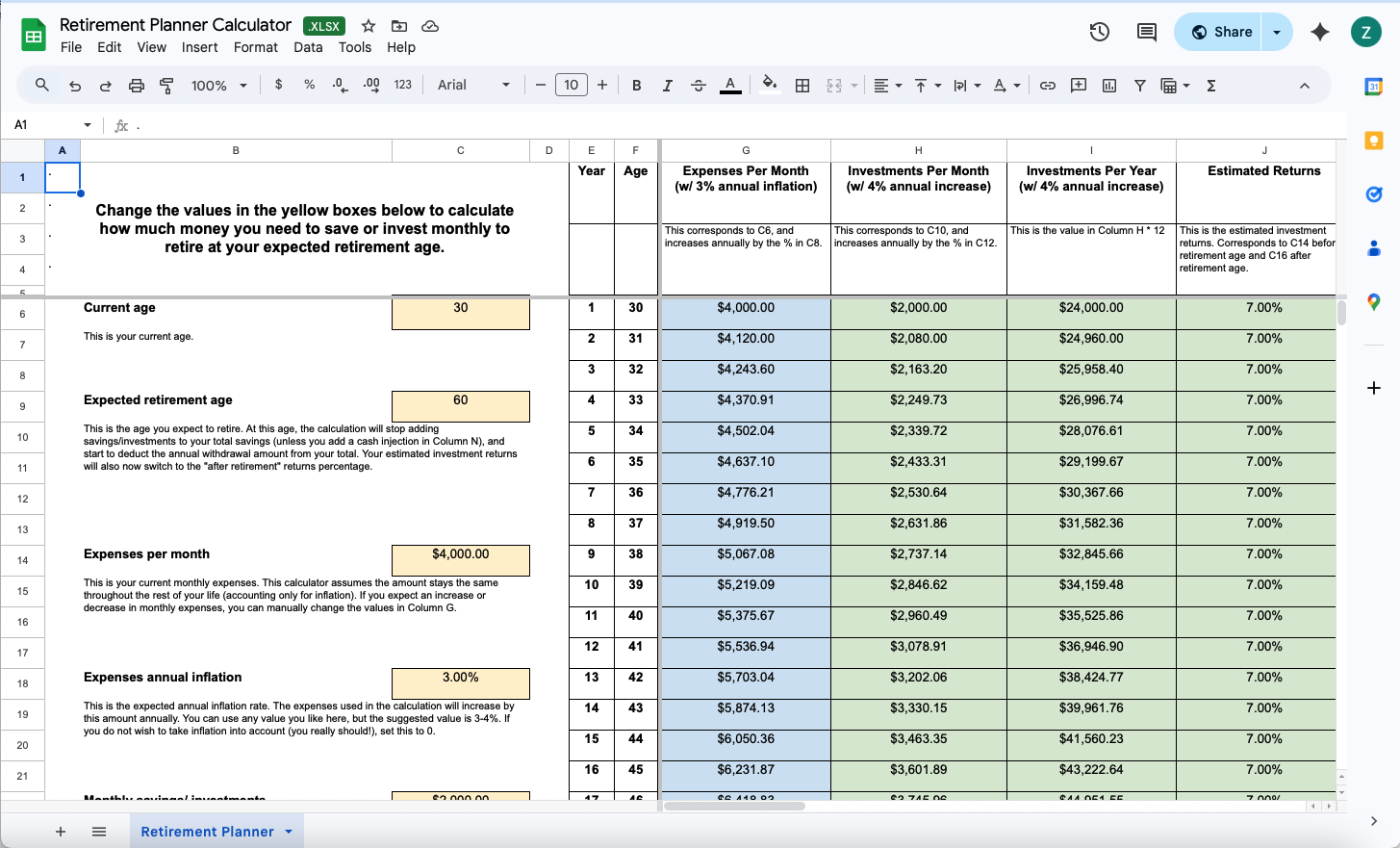
Below is an example:
Therefore, for a patient with these two multiple primary cancers, the maximum reimbursement from her insurer would be $16,000/month.
Even with this additional regulation for multiple primary cancers, only the cost of the highest drug would be covered for each primary cancer treatment.
Hence, we can expect some out-of-pocket expenses if we exceed the claim limits.
From all these changes, we observe three things:
- The cost of medical treatment, especially for cancer treatment, has increased. Thus, MOH instituted this capped limit to reduce the cost of cancer treatment for public health.
- More people are detecting cancer due to regular screening, which increases the demand and cost of cancer treatment.
- The government may continue to make more changes in the future, which means patients may bear more of their treatment costs due to increasing limitations on hospital insurance coverage.
This further reminds us of the importance of having personal life insurance coverage, especially for critical illnesses. If you are concerned about covering potential shortfalls caused by coverage limitations, you may consider standalone cancer plans (i.e Income Complete Cancer Cover, Chinalife Cancer Guardian) that pay out a lump sum of money upon early or late-stage cancer diagnosis.
Such solutions are lower in cost. For a 30-year-old male, a $100,000 lump sum coverage would cost only $18.70 per month. For a 30-year-old female, it would only cost $40.10 per month.
If you are open to hearing more, please let me know via WhatsApp or simply reply to this email.
Have a great week ahead!
Best Regards,